Anal pain, (pain in the bottom) is common. There are things you can do to ease it but see a doctor if you’re in a lot of pain or it does not get better. Anal pain has many different causes. Your symptoms might give you an idea of what is causing anal pain.
Anal pain, which is pain in or around your bottom (anus) or back passage (rectum), is also known as proctalgia. It is a common complaint that can affect anyone, at any age.
Anal pain is often caused by a minor condition and often goes away on its own. You can usually relieve the pain yourself but if not, your GP will be able to offer treatment.
Causes of anal pain
Anal pain causes include:
- Anal abscess — a painful swelling containing infected liquid (pus) with swelling and redness, which is caused by an infection in or around your anus; treatments include:
- Antibiotics – if the abscess is caught early
- Draining of the abscess – this may need to be carried out at the hospital under general anaesthetic
- Anal fissure — a tear in the skin tissue that lines the opening of your bottom, which usually heals on its own after a few weeks and causes sharp, severe anal pain after a bowel movement or a burning pain that lasts for several hours after a bowel movement, as well as bleeding from your back passage; treatments include:
- Drinking more fluids, eating a diet high in fibre and taking laxatives — anal fissures can be caused by passing a large or hard stool; these approaches will soften your stools
- Ointment to relax the ring of muscle around your anus
- Over-the-counter painkillers
- Surgery to help your anal fissure heal
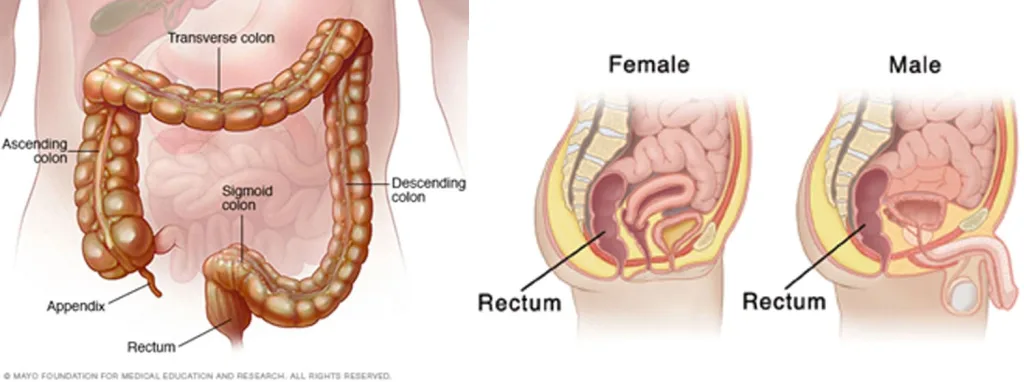
- Anal fistula — an infected tunnel that develops between your anus and your rectum that develops from an anal abscess and causes throbbing, constant pain, swelling and itchy skin around your anus, bleeding from your anus and a high temperature (fever); treatment almost always involves anal fistula surgery
- Haemorrhoids (piles) — piles do not always cause symptoms but if they do, symptoms often resolve after a few days and include swellings inside or around your anus, an itchy anus, soreness, redness and bleeding after passing a stool; treatments include:
- Drinking more fluids, eating a diet high in fibre and taking laxatives — piles can be caused by straining when having a bowel movement due to constipation; these approaches will soften your stools
- Over-the-counter painkillers
- Surgery — if the blood supply to the pile is blocked by a clot, surgery under local anaesthetic can be carried out to remove the clot
Occasionally, other anal pain causes include:
- A urinary tract problem
- Anal sex
- Coccydynia — a painful tail bone
- Digestive system symptoms and conditions — this includes constipation, Crohn’s disease and diarrhoea
- Infections — this includes:
- Fungal infections
- Sexually transmitted infections (STIs) — this includes anogenital warts, which you may see or feel as bumps around your anus, and herpes, which causes anal pain with blisters or a blistery rash
- Some rare cancers eg cancer of the anus or rectum — anal pain is usually constant and worse when you have a bowel movement; other symptoms include blood mixed with your stools or on your underwear
Rectal prolapse can also cause anal pain. This occurs when muscles that support your back passage weaken, allowing some of your rectum to bulge out of your anus. Symptoms include difficulty holding your stools in and feeling a lump in your anal area.
If all other causes have been ruled out, you may receive one of two diagnoses:
- Levator ani syndrome — a constant or long-lasting achy or pressured feeling in and around your anus, which is worse when sitting and affects six in every 100 people, often having a significant impact on their quality of life; physiotherapy to relax your pelvic muscles can help
- Proctalgia fugax — this common condition affects up to one in every five people and involves sudden, severe bouts of anal pain that last for several seconds or minutes at a time; medicines to relax your pelvic muscles can help
It is not fully understood what causes levator ani syndrome or proctalgia fugax. Spasms of the muscles around the anus may be involved but it is not known what triggers these spasms. These conditions are more common in people with anxiety or irritable bowel syndrome (IBS).
Anal pain can affect the area in or around your bottom (anus) or back passage (rectum). Anal pain is sometimes accompanied by rectal bleeding and can be distressing.
| Symptoms | Possible cause |
|---|---|
| Pooing less than normal for you and pain when pooing | Constipation |
| Itchy anus, feeling a lump around the anus, blood on the paper after wiping | Piles (haemorrhoids) |
| Sharp pain when pooing, burning pain after doing a poo and blood on the paper after wiping | Anal fissures |
| Constant throbbing pain, pus and blood on the paper after wiping, high temperature | Anal fistulas and abscesses |
Less often, anal pain can be caused by something else like a sexually transmitted infection (STI) or fungal infection. Rarely, it can be a sign of something serious like anal cancer.
How you can ease or prevent anal pain
Do
- drink lots of fluid and eat plenty of fibre to keep your poo soft
- exercise regularly
- wipe your bottom with damp toilet paper
- take paracetamol
- take a warm bath to ease itching and pain
- put an ice pack (or bag of frozen peas) in a towel on the painful area for up to 20 minutes every 2 to 3 hours
Don’t
- do not scratch around your anus
- do not ignore the urge to poo
- do not push too hard when pooing
- do not use fragranced products, such as shower gels or soaps around your anus
- do not eat spicy food or drink alcohol and caffeine
- do not lift or carry anything heavy
- do not take ibuprofen if your anus is bleeding
A pharmacist can help with anal pain
A pharmacist can recommend medicines to reduce constipation and anal pain such as:
- painkillers like ibuprofen or paracetamol
- creams or suppositories (medicines you put into your bottom) to ease itching, pain and swelling
- medicines that help make it easier to poo (laxatives)
Many pharmacies have private areas if you do not want to be overheard.
Treatment for anal pain
Treatment for anal pain depends on what’s causing it.
A GP will examine you and may prescribe:
- a cream or ointment to ease your pain
- laxatives to help you poo more easily
- antibiotics if you have an infection
The GP may also recommend changes to your diet or arrange for tests to look for a cause of the anal pain.
Sometimes surgery or other treatments may be needed if the pain is caused by severe anal fissures, piles or fistulas.
